The American College of Cardiology (ACC) has declared a cardiology workforce crisis. Driven by rising patient demand and a fixed, insufficient pipeline of graduating fellows.
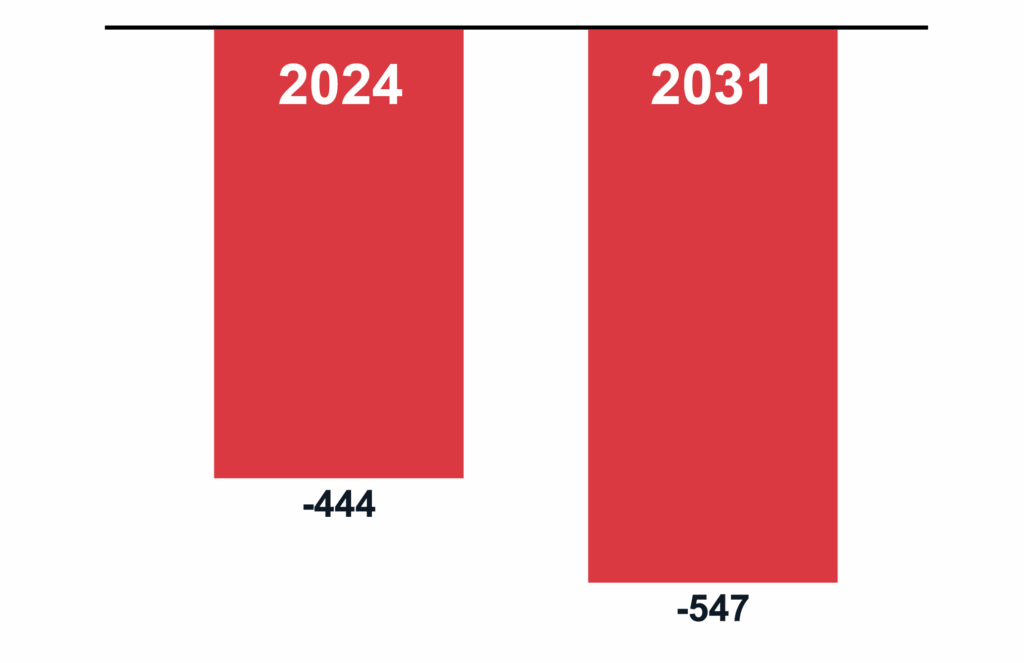
The deficit is real, and while the cardiologist shortage is not a new concept, the projections are worsening. The field loses a net of 450 cardiologists annually, a trend expected to reach nearly 550 by 2031 (Figure 1).
In the setting of an aging population and a projected 30% increase in heart disease prevalence by 2060, the workforce gap leaves too few clinicians to meet growing needs.
Further underscoring the crisis, the AMA estimates that one in five doctors plans to exit the workforce within the next two years. In cardiology, this imbalance may be even more profound: 25% of practicing cardiologists are nearing retirement age.
Projected Net Annual Loss of Cardiologists
Call Coverage & Burnout: The Pressure Points
During their career, all cardiologists shoulder night and weekend call duties in addition to their daytime responsibilities. While a vital component of patient care, call is widely regarded as one of the least desirable aspects of practice. Surveys confirm this sentiment: more than 50% of cardiologists would accept lower pay in exchange for reduced call obligations.
The pressure points are clear:
- Aging workforce: Call participation naturally declines over a cardiologist’s career. While many senior physicians prefer to remain active, some can no longer manage the physical demands of a full weekend of call. Whether by choice or necessity, 30% of cardiologists over age 60 exit the call schedule, leaving the remaining burden to be redistributed among fewer clinicians.
- Younger workforce expectations: Ninety percent of younger generation physicians report that work-life balance is a key factor in their job selection, with call schedules being a significant consideration in those decisions.
- Unsustainable demand: With patient volumes climbing and fewer clinicians to absorb the load, more than 50% of cardiologists report burnout, with call obligations as a leading contributing factor. Burnout erodes physician well-being, disrupts patient access, and complicates health system recruitment and retention.
Table 1: Burnout Rates and Call Participation by Career Stage
Table 1. Burnout and Call Participation Across Career Stages.
Burnout rates increase from 10% during fellowship to 39% in mid-career, while call participation decreases with advancing career stage.Mid-career defined as 8–21 practice years; late career defined as >61 years of age. Sources: JACC 2019,5 ACC 2020.6<
/p>
Career Stage |
Burnout Rates (%) |
Call Participation (%) |
|---|---|---|
Fellowship |
10 |
100 |
Early Career |
23 |
89–93 |
Mid-Career* |
39 |
89 |
Late Career† |
28 |
70 |
*Defined as 8–21 practice years; †Defined as >61 years of age. 1. Shanafelt TD, West CP, Sinsky C, et al. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General Population. J Am Coll Cardiol. 2019;73(17):2195–2211. doi:10.1016/j.jacc.2019.04.031 2. The Vexing Challenge of Physician Slowdown: How to Create an Effective Policy. American College of Cardiology. Published September 1, 2020. Available at:
www.acc.org/Latest-in-Cardiology/Articles
The Cardiology Call Crisis → Call Solutions
The Role of Advanced Practice Providers (APPs)
Expanding the use of nurse practitioners and physician assistants can buffer call schedules, especially in busy programs, but their roles remain limited.
- Scope constraints: APP authority varies by state and hospital bylaws, and these providers typically require physician backup. High-acuity areas, such as the emergency departments and Intensive Care Units, often necessitate direct physician coverage and communication.
- Specialty Training: A non-invasive cardiologist completes at least six years of postgraduate training in internal medicine and cardiology subspecialty care. Their expertise in managing complex cardiovascular cases cannot be substituted by the generalist training path of an APP, who typically specializes through on-the-job experience rather than formal residency and fellowship programs.
- Practice reality (limitations): In many cardiology practices, the majority of APP work remains outpatient-focused. While their roles are expanding to support acute-care settings, published data on APP participation in night and weekend call remains limited. This suggests that while APPs can effectively buffer daytime workloads, they are less likely to absorb overnight call burdens.
Pipeline Expansion
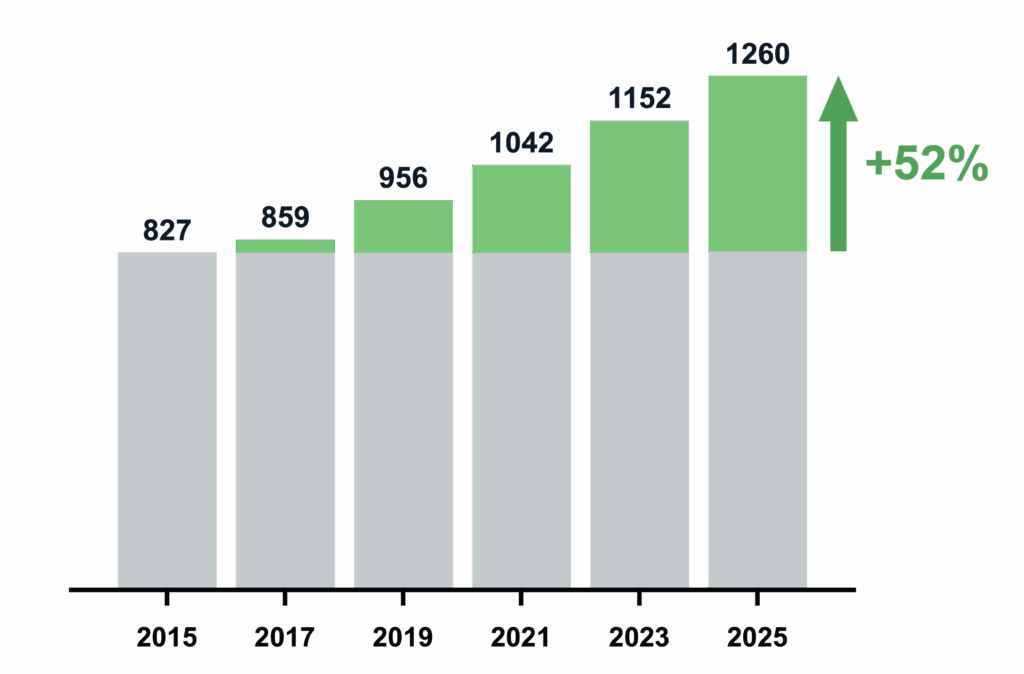
The American College of Cardiology (ACC) has been working diligently to strengthen and expand trainee programs, advocating for more GME funding and launching initiatives such as the Emerging Faculty Leadership Academy. Fellowship positions have increased steadily over the last decade, rising by more than 50%, from 827 in 2015 to 1,260 in 2025 (Figure 3). While this builds long-term capacity, it does not address the immediate call burden on today’s cardiologists practicing outside of academic institutions.
Growth in Matched Cardiology
Fellowship Positions 2015-2025
Rewriting Schedules for Call Relief and Rest
“The responsibility is on the practice to find ways in which they can allow doctors to take care of their patients at night, yet preserve their best resource to really provide care to patients during the day.” — Dan Bensimhon, M.D., F.ACP, Director Advanced Heart Failure, Cone Health
A more direct solution involves expanding the physician call pool itself by utilizing board-certified cardiologists to cover weekend, night, and holiday shifts on a long-term, part-time basis. Night time work is imperative for patient care, but represents the least productive hours of the day. This model allows employed cardiologists time to rest, minimizes the loss of productivity associated with post-call recovery, and enhances focus on daytime care.
This approach was first introduced to the market in 2007. Unlike traditional locums, who rotate through short assignments with limited continuity, moonlighting physicians function as a consistent extension of the call team. Many bring an academic approach to care, with 85% maintaining academic affiliations.
Benefits of a Moonlighter-Led Call Relief Program™ include:
- Physician Well-Being: Reduced call frequency can contribute to lower burnout and improve work-life balance.
- Patient Access: Rested physicians no longer require post-call recovery days and are available for procedural and outpatient responsibilities.
- Dedicated Availability and Coverage:Moonlighting physicians choose to cover nights or weekends rather than absorbing it on top of existing duties. They bring focused attention and fresh energy to shifts that are otherwise considered the most taxing.
- Recruitment and Retention: More manageable call schedules are a strong recruiting tool and also help retain experienced staff and delaying retirement.
-
Capturing Missed Revenue: Although upfront costs exist, reduced turnover, enhanced productivity, and decreased reliance on traditional locum tenens services offset these expenses.
Conclusion and a Plan for Action
The cardiology call crisis accentuates the widening gap between rising patient demand and the realities of an overburdened physician workforce. Traditional non-invasive call structures, which were designed for a different era of medicine, are no longer sustainable. Burnout, retirement, and a shift in workforce expectations mean that without some intervention, such as revising call schedules, health systems risk losing talent and compromising patient access.
The good news is that practices do not need to wait for new fellows to enter the workforce. Rethinking call coverage at the local level is a great first step. A Moonlighter-Based Call Relief Program can protect employed physicians, sustain high-quality patient care, and help a practice gain a competitive edge in recruitment and retention.
The good news is that practices do not need to wait for new fellows to enter the workforce. Rethinking call coverage at the local level is a great first step. A Moonlighter-Based Call Relief Program can protect employed physicians, sustain high-quality patient care, and help a practice gain a competitive edge in recruitment and retention.
Action Steps for Cardiology Practices
1. Audit Call Schedules
- ✓ This might sound basic, but not leave physicians to fill call gaps on their own. Map out current call participation by age, subspecialty, and workload (e.g., whether interventional cardiologists or EPs are participating in non-invasive call, and how this impacts daytime productivity).
- ✓ Identify trends in your cardiology practice such as senior physicians exiting call, to anticipate and prevent future coverage gaps.
2. Engage Physicians in Honest Dialogue
- ✓ Survey employed cardiologists on their willingness to trade compensation for reduced call; consider a cost-sharing model for practice buy-in.
- ✓ Survey employed cardiologists on their willingness to trade compensation for reduced call; consider a cost-sharing model for practice buy-in.
- ✓ Discuss retirement timelines proactively.
3. Leverage APPs Strategically
- ✓ If not already involved, include APPs in call schedules as buffers for physicians, focusing on taking outpatient triage calls, and lower-acuity inpatient calls from medical wards.
- ✓ Avoid relying on APPs for high-acuity departments where physician expertise is required.
4. Explore Call Relief Partnerships
- ✓ Evaluate moonlighting or part-time call relief models to supplement weekend, night, and holiday shifts.
- ✓ Prioritize working with a partner that has experience onboarding a panel of board-certified, academic clinicians with a track record of placing their physicians into longer-term assignments.
5. Reframe Recruitment Messaging
- ✓ Treat call relief and physician wellness as a benefit to your doctors, not a one-time fix.
- ✓ Advertise call schedules as part of your hiring package. A lot of practices are listing high-paying non-invasive cardiology positions, but very few are investing in Call Relief.
- ✓ Position innovative call solutions as a differentiator for attracting fellows and early-career cardiologists.
6. Monitor and Adjust
- ✓ Track burnout, retention, and patient access metrics before and after implementing changes.
- ✓ Partner with organizations experienced in physician wellness to assist with tracking program success.
Partnering for Sustainable Call Coverage: Key Questions to Ask
If you’re considering external support for night and weekend call, the right partner shouldn’t feel like a staffing agency. They should function as a strategic extension of your team.
- Work exclusively with board-certified or board-eligible cardiologists
- Demonstrate a deep understanding of the physician wellness space
- Operate a dedicated program focused on consistent, high-quality call relief rather than traditional locums coverage
Physicians who thrive in recurring call roles are not the same as those rotating through short-term assignments. The best partners recognize this distinction and build their models accordingly.
- What is your track record in staffing recurring call coverage programs?
- How do you model the panel size required for sustainable coverage, accounting for frequency, call volumes, and local physician availability?
- How does the structure of our cardiology weekend call impact the candidate pool?
- Do you have specific expertise in cardiology call coverage, or is your model generalized across multiple specialties?
- How do you monitor the well-being of our employed cardiologists during the coverage programs?
- Have you published or contributed to the field of physician burnout or patient access?
These questions will help you separate transactional vendors from long-term clinical partners. In today’s landscape, cardiology practices need the latter.
References
- 2024 Cardiovascular Workforce Data. MedAxiom; 2024. Available at: https://medaxiom.com.
- American College of Cardiology. Projected Cardiology Workforce Losses, 2031. ACC; 2024. Available at: https://www.acc.org.
- Amin A, Sinha SS, Wong C, et al. Match Outcomes for Cardiovascular Disease Fellowship Training, 2010 to 2021. ResearchGate. 2022. Available at: https://www.researchgate.net/publication/366410439_Match_Outcomes_for_Cardiova scular_Disease_Fellowship_Training_2010_to_2021
- National Resident Matching Program (NRMP). Specialties Matching Service Results and Data, 2025 Appointment Year. Washington, DC: NRMP; 2025. Available at: https://www.nrmp.org/wp-content/uploads/2025/02/SMS_Results_and_Data_2025.pdf
- Shanafelt TD, West CP, Sinsky C, et al. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General Population. J Am Coll Cardiol.2019;73(17):2195–2211. doi:10.1016/j.jacc.2019.04.031
- American College of Cardiology. The Vexing Challenge of Physician Slowdown: How to Create an Effective Policy. American College of Cardiology. Published September 1, 2020. Available at: https://www.acc.org/Latest-in-Cardiology/Articles/2020/09/01/01/42/The-Vexing-Challenge-of-Physician-Slowdown-How-to-Create-an-Effective-Policy